1.1.3 X-ray Imaging
"I have seen my death." — Anna Bertha Röntgen, December 22, 1895
🎯 An Accidental Discovery That Changed Medicine
The Night That Changed the World
On November 8, 1895, Wilhelm Conrad Röntgen, a physics professor at the University of Würzburg in Germany, was studying cathode rays in his laboratory. It was already evening, and the laboratory was pitch dark, with only the faint glow from the cathode ray tube.
Röntgen completely wrapped the cathode ray tube in black cardboard, ensuring no visible light leaked out. But when he turned on the power, something unexpected happened: a fluorescent screen coated with barium platinocyanide several meters away emitted a faint green glow!
This couldn't be cathode rays—cathode rays can only travel a few centimeters in air. It must be some unknown ray that penetrated the black cardboard. Röntgen named this mysterious ray "X-rays," with X representing "unknown."
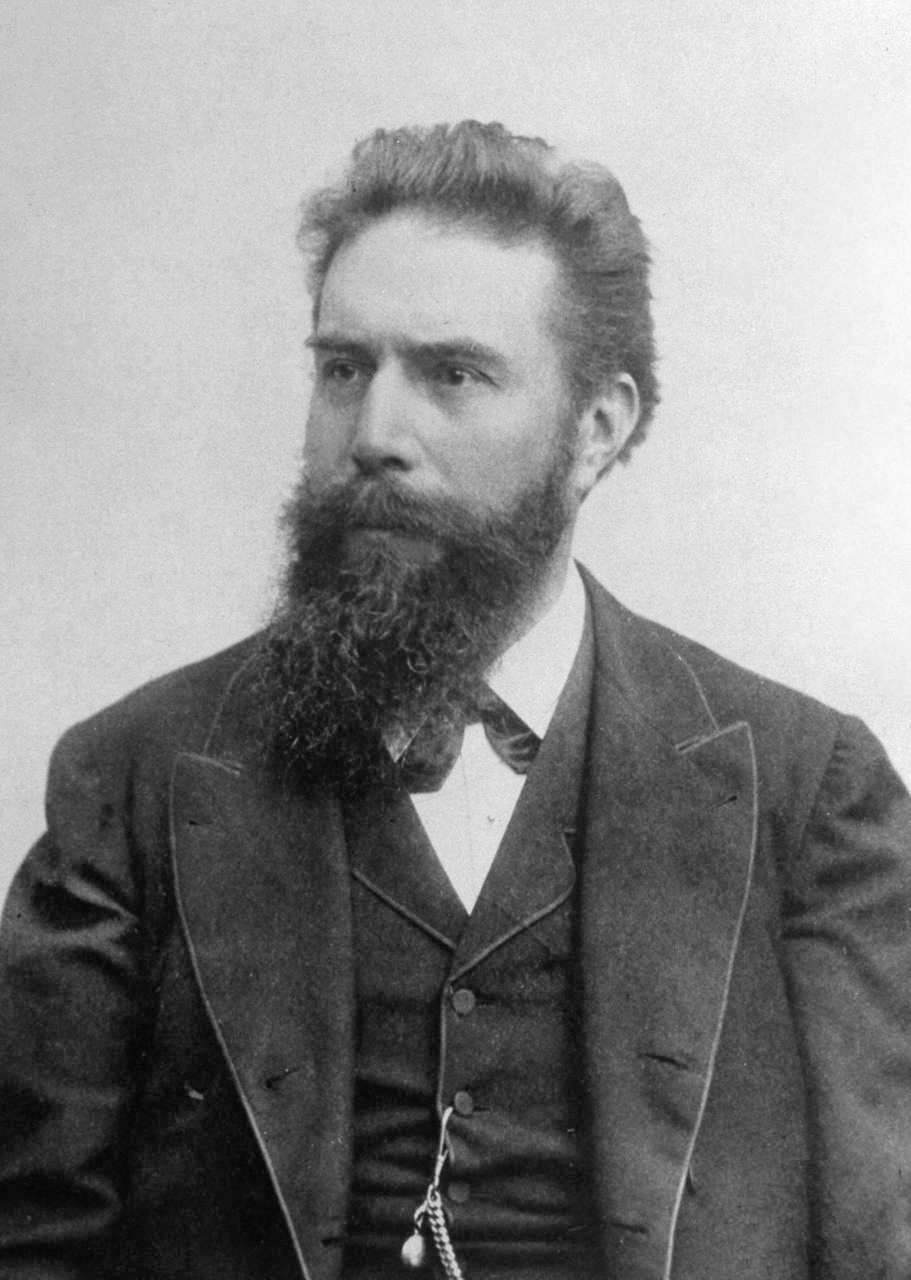 Wilhelm Conrad Röntgen, discoverer of X-rays
Wilhelm Conrad Röntgen, discoverer of X-rays
💡 Why Called "X"-rays?
In mathematics, X typically represents an unknown variable. Röntgen used "X" to name this mysterious ray, indicating he didn't know what it was at the time. Although scientists later understood the nature of X-rays (high-energy electromagnetic waves), the name "X-rays" has persisted. In Germany and some European countries, X-rays are also called "Röntgen rays" to honor the discoverer.
The First X-ray Image: His Wife's Hand
Over the following weeks, Röntgen worked day and night studying this mysterious ray. He discovered:
- X-rays can penetrate wood, paper, and cloth
- X-rays can expose photographic plates
- X-rays cannot penetrate metal and bone
On December 22, 1895, Röntgen conducted a bold experiment: he had his wife Anna Bertha place her hand on a photographic plate, then exposed it to X-rays for 15 minutes. When the plate was developed, a shocking image appeared: clear hand bones and a wedding ring!
This was the first X-ray medical image in human history. It is said that when Anna Bertha saw the image of her hand bones, she exclaimed: "I have seen my death!"
📸 A Historic Moment
This photograph not only marked the beginning of medical imaging but also signified the first time humans could "see" internal structures without cutting open the body. Before this, doctors could only infer internal conditions through palpation, percussion, and auscultation, or observe directly through surgery. The discovery of X-rays completely changed this.
Rapid Spread of X-rays
Röntgen submitted his first paper "On a New Kind of Rays" to the Würzburg Physical-Medical Society on December 28, 1895. The news quickly spread worldwide:
- January 1896: Newspapers in Vienna, London, and New York competed to report
- February 1896: American doctors first used X-rays to diagnose fractures
- March 1896: X-rays began being used to diagnose battlefield casualties
- End of 1896: Thousands of X-ray devices were already in use worldwide
This speed of dissemination was unprecedented at the time. The discovery of X-rays was not only a scientific breakthrough but also a medical revolution.
First Nobel Prize in Physics
In 1901, the Nobel Prize was awarded for the first time, and Röntgen received the first Nobel Prize in Physics for discovering X-rays. This was the highest recognition of his pioneering work.
Interestingly, Röntgen refused to patent X-rays, believing this discovery should belong to all humanity and anyone should be able to use it freely. He donated all his Nobel Prize money to the University of Würzburg.
⚠️ The Cost of Early X-rays
In the first few years after X-ray discovery, people didn't understand the dangers of radiation. Many early X-ray pioneers, including Röntgen's assistants and many doctors, developed radiation sickness from prolonged X-ray exposure, even losing fingers or their lives. It wasn't until the early 20th century that people gradually recognized the importance of radiation protection.
🔬 How Do X-rays "See" the Human Body?
The Nature of X-rays
X-rays are a type of high-energy electromagnetic wave, belonging to the same family as visible light and radio waves, but with much higher energy:
- Wavelength: 0.01-10 nanometers (visible light wavelength is about 400-700 nanometers)
- Frequency: 30 PHz - 30 EHz (1 PHz = 10¹⁵ Hz)
- Energy: 100 eV - 100 keV (medical X-rays typically 20-150 keV)
It is precisely this high energy that enables X-rays to penetrate human tissue.
X-ray Generation: The X-ray Tube
The basic principle of modern X-ray tubes is similar to Röntgen's era, but the technology has greatly improved:
Working Principle:
- Cathode Heating: Tungsten filament cathode is heated to about 2000°C, releasing large numbers of electrons
- High Voltage Acceleration: Electrons are accelerated under high voltage (typically 40-150 kV)
- Anode Impact: High-speed electrons strike the tungsten or molybdenum anode target
- X-ray Production: Electron kinetic energy converts to X-rays (about 1%) and heat (about 99%)
💡 Why Are X-ray Tubes So Hot?
X-ray production efficiency is very low, with only about 1% of electron energy converting to X-rays, with the remaining 99% becoming heat. This is why X-ray tubes need powerful cooling systems, typically using oil or water cooling. In early days, X-ray tubes often failed due to overheating.
X-ray Interactions with Matter
When X-rays pass through the human body, three main interactions occur:
1. Photoelectric Effect
- X-ray photon is completely absorbed by an atom
- Mainly occurs in high atomic number materials (such as calcium in bones)
- This is the main source of X-ray imaging contrast
2. Compton Scattering
- X-ray photon collides with electron, changing direction and energy
- Reduces image contrast, produces noise
- Requires use of collimators and anti-scatter grids to reduce scattering
3. Coherent Scattering
- X-ray photon changes direction but doesn't lose energy
- Has minor impact in medical imaging
X-ray Attenuation in Different Tissues
Different tissues have different X-ray absorption capabilities, which is the basis of X-ray imaging:
| Tissue Type | Relative Attenuation | X-ray Image Appearance | Typical Application |
|---|---|---|---|
| Air | Very Low | Black (high transmission) | Lung imaging |
| Fat | Low | Dark gray | Soft tissue contrast |
| Soft Tissue/Water | Medium | Gray | Organ imaging |
| Bone | High | Light gray/white | Fracture diagnosis |
| Metal | Very High | White (low transmission) | Implants, foreign bodies |
📊 Attenuation Coefficient and Atomic Number
Tissue X-ray attenuation capability mainly depends on:
- Atomic Number: Higher atomic number, stronger absorption (calcium atomic number is 20, much higher than hydrogen, carbon, oxygen)
- Density: Greater density, stronger absorption
- X-ray Energy: Higher energy, stronger penetration
This is why bones (containing calcium) appear white in X-ray images, while lungs (filled with air) appear black.
Traditional Film Imaging vs. Digital Imaging
Traditional Film Imaging (1895-1980s):
- X-rays directly expose photographic film
- Requires darkroom development
- Cannot adjust contrast and brightness
- Inconvenient storage and transmission
Digital Imaging (1980s-present):
- Computed Radiography (CR): Uses imaging plate (IP) to store X-ray information, then laser scans to read
- Digital Radiography (DR): Uses flat-panel detector to directly convert X-rays to digital signal
- Can adjust window width and level
- Convenient for storage, transmission, and post-processing
Relationship Between X-ray Imaging and CT
X-ray imaging and CT both use X-rays, but the imaging methods are completely different:
| Feature | X-ray Imaging | CT |
|---|---|---|
| Imaging Method | Projection imaging (2D) | Tomographic imaging (3D) |
| X-ray Source | Fixed position | Rotating scan |
| Image Reconstruction | Direct imaging | Requires complex algorithms |
| Radiation Dose | Low (0.01-0.1 mSv) | Higher (1-10 mSv) |
| Depth Information | None (all structures overlapped) | Yes (layer-by-layer display) |
| Typical Applications | Fractures, lungs, chest | Complex lesions, tumors |
💡 A Vivid Analogy
X-ray imaging is like photographing a book, with all pages overlapping—you can only see a flat shadow. CT is like scanning the book page by page—you can see the content of each page. X-ray imaging is fast, simple, with low radiation dose, suitable for initial screening; CT provides more detailed information but requires more time and radiation dose.
📈 Evolution of X-ray Technology
Technology Evolution Timeline
| Era | Milestone Events | Key Technologies | Imaging Time | Main Applications |
|---|---|---|---|---|
| 1895-1900s | X-ray discovery & early application | Cathode ray tube, film | Minutes | Fractures, foreign bodies |
| 1895: Röntgen discovered X-rays | ||||
| 1896: First medical application | ||||
| 1901: Röntgen received first Nobel Prize in Physics | ||||
| 1900s-1950s | Film era | Improved X-ray tubes, intensifying screens | Seconds | Chest, bones, gastrointestinal |
| Film quality improved | ||||
| Contrast agent application | ||||
| 1950s-1980s | Image intensifier era | Image intensifier, fluoroscopy | Real-time | Interventional surgery, angiography |
| 1950s: Image intensifier introduced | ||||
| Real-time fluoroscopy became possible | ||||
| 1980s-1990s | Digital beginning | Computed Radiography (CR) | Seconds | All body parts |
| 1981: Fuji launched first CR system | ||||
| Images can be digitally stored and transmitted | ||||
| 1990s-2000s | Flat-panel detector revolution | Digital Radiography (DR) | <1 second | All body parts, mobile X-ray |
| Late 1990s: First DR system | ||||
| Image quality greatly improved | ||||
| 2010s-present | Intelligence & low dose | Dual-energy imaging, tomosynthesis, AI | <1 second | Precise diagnosis, low-dose screening |
| Digital Breast Tomosynthesis (DBT) | ||||
| AI-assisted diagnosis |
Key Technology Breakthrough Comparison
| Technology Category | Technology Name | Time | Core Contribution | Performance Improvement |
|---|---|---|---|---|
| Detector | Film + intensifying screen | 1900s | Improve photosensitivity | Exposure time from minutes to seconds |
| Real-time Imaging | Image intensifier | 1950s | Real-time fluoroscopic imaging | Enable dynamic observation and interventional surgery |
| Digitization | Computed Radiography (CR) | 1981 | Imaging plate replaces film | Digital storage, adjustable window width/level |
| Digitization | Digital Radiography (DR) | Late 1990s | Flat-panel detector direct conversion | Image quality improved, instant imaging |
| Advanced Imaging | Dual-energy imaging | 2000s | Two energy X-rays | Tissue separation, bone removal |
| Advanced Imaging | Digital Breast Tomosynthesis (DBT) | 2010s | Multi-angle projection reconstruction | Pseudo-3D imaging, reduce tissue overlap |
| Dose Optimization | Automatic Exposure Control (AEC) | 1980s-1990s | Real-time adjust exposure parameters | Radiation dose reduced 30-50% |
| AI Assistance | Deep learning diagnosis | 2010s | Automatic lesion detection | Improve diagnostic accuracy and efficiency |
🎯 From Film to Digital: A Revolution
The transition from film to digital was not just technological progress, but a workflow revolution:
- Film Era: Shoot → darkroom development (15-30 minutes) → view → archive (occupies large physical space)
- Digital Era: Shoot → instant display (<10 seconds) → adjust parameters → electronic archive → remote transmission
Digitization made remote consultation and AI-assisted diagnosis possible, greatly improving medical efficiency.
CR vs. DR Technology Comparison
| Feature | Computed Radiography (CR) | Digital Radiography (DR) |
|---|---|---|
| Launch Time | 1981 (Fuji) | Late 1990s |
| Detector | Imaging Plate (IP) | Flat-Panel Detector (FPD) |
| Workflow | Exposure → remove IP → scan read | Exposure → instant display |
| Imaging Time | Seconds (requires scanning) | <1 second (instant) |
| Image Quality | Good | Excellent |
| Spatial Resolution | 2.5-5 lp/mm | 3-7 lp/mm |
| Dynamic Range | 10,000:1 | 10,000:1 |
| Radiation Dose | 30-50% lower than film | 20-30% lower than CR |
| Cost | Medium | Higher |
| Portability | Better (IP movable) | Average (detector heavier) |
| Typical Applications | Routine X-ray examinations | High-end hospitals, emergency, ICU |
Modern X-ray Technology Innovations
1. Dual-Energy Imaging
- Uses two different energy X-rays
- Can separate different tissues (such as bone and soft tissue)
- Applications: Chest imaging with rib removal, gout crystal detection
2. Digital Breast Tomosynthesis (DBT)
- Acquires projection images from multiple angles
- Reconstructs into pseudo-3D images
- Applications: Breast cancer screening, reduce false positives
3. Mobile X-ray
- Portable DR systems
- Can be used at bedside, operating room, emergency room
- Applications: ICU patients, intraoperative imaging
4. AI-Assisted Diagnosis
- Automatically detect lung nodules, fractures, pneumothorax, etc.
- Assist doctors in improving diagnostic accuracy
- Reduce missed and misdiagnoses
🤖 AI Applications in X-ray Diagnosis
In recent years, deep learning has made significant progress in X-ray image analysis:
- Lung Nodule Detection: Sensitivity can reach over 95%
- Fracture Detection: Accuracy exceeds human doctors in some areas (such as carpal bones)
- COVID-19 Screening: Rapidly identify lung infection characteristics
However, AI is currently still an assistive tool, with final diagnosis requiring doctor confirmation.
🎯 Clinical Significance of X-ray Technology Evolution
Each advancement in X-ray technology has greatly improved clinical diagnosis and patient experience:
| Evolution Dimension | Early X-ray | Modern X-ray | Clinical Significance |
|---|---|---|---|
| Imaging Speed | Minutes | <1 second | From "static posing" to "instant imaging" |
| Image Quality | Blurry, low contrast | Clear, high contrast | From "barely visible" to "precise diagnosis" |
| Radiation Dose | High (no protection awareness) | Low (ALARA principle) | From "radiation injury" to "safe examination" |
| Application Scope | Fractures, foreign bodies | All body systems | From "limited application" to "widespread screening" |
| Workflow | Film development, physical archiving | Digital, remote transmission | From "cumbersome inefficient" to "fast convenient" |
⚠️ Radiation Dose and Safety
Although modern X-ray technology has greatly reduced radiation dose, radiation risk still exists. Understanding radiation doses for different examinations is important:
| Examination Type | Typical Effective Dose | Equivalent Natural Background Radiation |
|---|---|---|
| Chest X-ray (PA) | 0.02 mSv | 3 days |
| Chest X-ray (Lateral) | 0.08 mSv | 12 days |
| Abdominal X-ray | 0.7 mSv | 4 months |
| Pelvis X-ray | 0.6 mSv | 3 months |
| Lumbar Spine X-ray | 1.5 mSv | 7 months |
| Mammography | 0.4 mSv | 2 months |
ALARA Principle (As Low As Reasonably Achievable):
- Only perform X-ray examinations when necessary
- Use the lowest radiation dose to obtain image quality needed for diagnosis
- Shield sensitive organs (such as gonads, thyroid)
- Pregnant women and children require special caution
💡 Key Takeaways
Historical Significance: Röntgen accidentally discovered X-rays on November 8, 1895, and received the first Nobel Prize in Physics in 1901. The discovery of X-rays pioneered medical imaging, enabling humans to "see" internal structures non-invasively for the first time.
Imaging Principle: X-rays are high-energy electromagnetic waves, and different tissues have different X-ray absorption capabilities (bone > soft tissue > air), producing contrast in X-ray images.
Technology Evolution: From early film imaging (minutes of exposure) to modern digital imaging (<1 second), from simple projection imaging to advanced technologies like dual-energy imaging and tomosynthesis, X-ray technology continues to advance.
Digital Revolution: The emergence of CR (1981) and DR (late 1990s) completely transformed X-ray imaging, achieving digital storage, instant imaging, remote transmission, and AI-assisted diagnosis.
Radiation Safety: Modern X-ray technology follows the ALARA principle, with radiation dose greatly reduced. However, careful use is still needed, especially for pregnant women and children. A chest X-ray's radiation dose is approximately equivalent to 3 days of natural background radiation.
💡 Next Steps
Now you understand the basic principles and technological evolution of X-rays. In Chapter 3, we will delve into the algorithmic principles of X-ray image reconstruction and enhancement. In Chapter 2, we will learn X-ray image preprocessing methods, including denoising, contrast enhancement, and other practical techniques.