5.2 Image Segmentation: U-Net and its Variants
"U-Net is not just a network architecture, but a revolutionary thinking in medical image segmentation—proving that carefully designed architectures can surpass brute-force training on large datasets." — — Ronneberger et al., "U-Net: Convolutional Networks for Biomedical Image Segmentation", MICCAI 2015
In the previous section, we learned how to preprocess medical images from different modalities into formats suitable for deep learning. Now, we enter the core task of medical image AI: image segmentation. The goal of image segmentation is to assign a class label to each pixel in an image, such as segmenting tumor and edema regions in brain MRI, or segmenting organs and vessels in CT.
In 2015, the U-Net architecture proposed by Ronneberger et al. completely revolutionized the medical image segmentation field. Its unique design philosophy and excellent performance made it the benchmark model for medical image segmentation, still widely used and improved today.
⚡ U-Net's Success in Medical Imaging
Special Challenges of Medical Image Segmentation
Compared to natural image segmentation, medical image segmentation faces unique challenges:
| Challenge | Natural Image Segmentation | Medical Image Segmentation | U-Net's Solution |
|---|---|---|---|
| Data Scarcity | Millions of labeled images | Usually only hundreds | Skip connections enhance feature transfer |
| Boundary Precision Requirements | Relatively relaxed | Sub-pixel level precision requirements | Multi-scale feature fusion |
| Class Imbalance | Relatively balanced | Lesion regions usually very small | Deep supervision techniques |
| 3D Structure Understanding | Primarily 2D | Need 3D context information | Extended to 3D versions |
U-Net's Revolutionary Design Philosophy
U-Net's success stems from three core design principles:
- Encoder-Decoder Structure: Compress information like a funnel, then gradually restore
- Skip Connections: Directly transfer shallow features to avoid information loss
- Fully Convolutional Network: Adapt to input images of any size
 U-Net's core idea: Encoder extracts semantic features, decoder restores spatial resolution, skip connections ensure details aren't lost - Custom diagram
U-Net's core idea: Encoder extracts semantic features, decoder restores spatial resolution, skip connections ensure details aren't lost - Custom diagram
🔧 U-Net Architecture Deep Dive
Basic U-Net Architecture
Let's deeply understand U-Net's network structure and data flow:
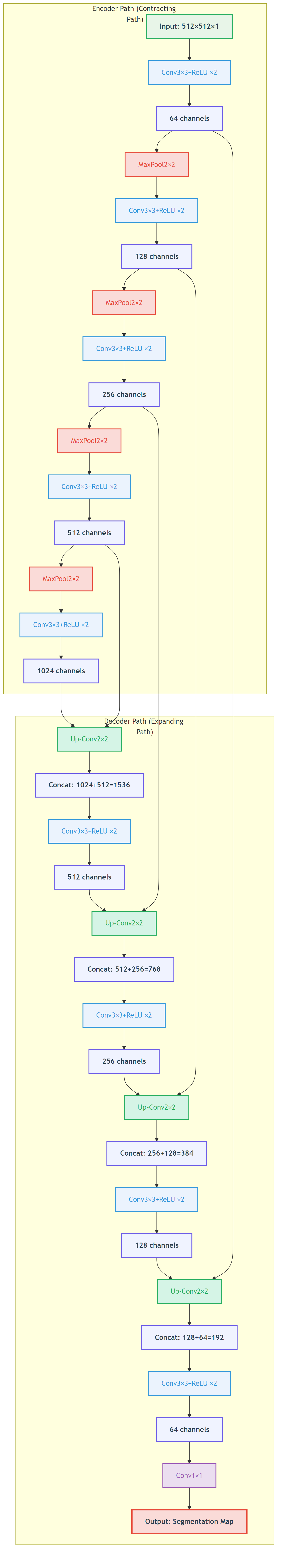 Figure: U-Net's encoder-decoder structure showing how skip connections transfer shallow features to deep layers to preserve spatial details.
Figure: U-Net's encoder-decoder structure showing how skip connections transfer shallow features to deep layers to preserve spatial details.
📖 View Original Mermaid Code
Detailed Analysis of Key Components
1. Encoder (Contracting Path)
The encoder's role is to extract multi-level features:
import torch
import torch.nn as nn
import torch.nn.functional as F
class EncoderBlock(nn.Module):
def __init__(self, in_channels, out_channels):
super().__init__()
self.conv1 = nn.Conv2d(in_channels, out_channels, 3, padding=1)
self.conv2 = nn.Conv2d(out_channels, out_channels, 3, padding=1)
self.pool = nn.MaxPool2d(2)
def forward(self, x):
x = F.relu(self.conv1(x))
x = F.relu(self.conv2(x))
return self.pool(x), x # Return pooled result and skip connection featuresEncoder characteristics:
- Increasing feature channels: 64 � 128 � 256 � 512 � 1024
- Decreasing spatial dimensions: Halved through 2�2 max pooling
- Expanding receptive field: Deeper features have larger receptive fields
2. Decoder (Expanding Path)
The decoder's role is to restore spatial resolution:
class DecoderBlock(nn.Module):
def __init__(self, in_channels, out_channels):
super().__init__()
self.upconv = nn.ConvTranspose2d(in_channels, out_channels, 2, stride=2)
self.conv1 = nn.Conv2d(out_channels * 2, out_channels, 3, padding=1) # Channels double after skip connection
self.conv2 = nn.Conv2d(out_channels, out_channels, 3, padding=1)
def forward(self, x, skip_connection):
x = self.upconv(x)
# Handle size mismatch
if x.shape != skip_connection.shape:
x = F.interpolate(x, size=skip_connection.shape[2:], mode='bilinear', align_corners=False)
x = torch.cat([x, skip_connection], dim=1) # Skip connection
x = F.relu(self.conv1(x))
x = F.relu(self.conv2(x))
return x3. Skip Connections
Skip connections are U-Net's core innovation:
Why are skip connections so important?
- Information Transfer: Directly transfer shallow spatial information
- Gradient Flow: Alleviate vanishing gradient problem
- Multi-scale Fusion: Combine high-level semantics with low-level details
def visualize_skip_connections():
"""
Visualize the role of skip connections
"""
import matplotlib.pyplot as plt
# Simulate feature maps
# Deep features: rich semantic information but low spatial resolution
deep_features = np.random.rand(8, 8) * 0.5 + 0.5
# Shallow features: rich spatial details but limited semantic information
shallow_features = np.random.rand(32, 32) * 0.3 + 0.2
fig, axes = plt.subplots(1, 3, figsize=(15, 5))
axes[0].imshow(deep_features, cmap='viridis')
axes[0].set_title('Deep Features (Semantics)')
axes[0].axis('off')
axes[1].imshow(shallow_features, cmap='viridis')
axes[1].set_title('Shallow Features (Details)')
axes[1].axis('off')
# Fusion effect visualization
fused = np.random.rand(32, 32) * 0.8 + 0.1
axes[2].imshow(fused, cmap='viridis')
axes[2].set_title('Skip Connection Fusion Result')
axes[2].axis('off')
plt.tight_layout()
plt.show()Complete U-Net Implementation
class UNet(nn.Module):
def __init__(self, in_channels=1, num_classes=2):
super().__init__()
# Encoder
self.enc1 = EncoderBlock(in_channels, 64)
self.enc2 = EncoderBlock(64, 128)
self.enc3 = EncoderBlock(128, 256)
self.enc4 = EncoderBlock(256, 512)
# Bottleneck layer
self.bottleneck = nn.Sequential(
nn.Conv2d(512, 1024, 3, padding=1),
nn.ReLU(),
nn.Conv2d(1024, 1024, 3, padding=1),
nn.ReLU()
)
# Decoder
self.dec4 = DecoderBlock(1024, 512)
self.dec3 = DecoderBlock(512, 256)
self.dec2 = DecoderBlock(256, 128)
self.dec1 = DecoderBlock(128, 64)
# Output layer
self.final_conv = nn.Conv2d(64, num_classes, 1)
def forward(self, x):
# Encoding process
x1, skip1 = self.enc1(x) # 64 channels
x2, skip2 = self.enc2(x1) # 128 channels
x3, skip3 = self.enc3(x2) # 256 channels
x4, skip4 = self.enc4(x3) # 512 channels
# Bottleneck layer
bottleneck = self.bottleneck(x4)
# Decoding process
x = self.dec4(bottleneck, skip4)
x = self.dec3(x, skip3)
x = self.dec2(x, skip2)
x = self.dec1(x, skip1)
# Final output
return self.final_conv(x)🚀 Key U-Net Variants
1. V-Net: 3D Medical Image Segmentation
Motivation for V-Net
Many medical images (like CT, MRI) are essentially 3D data, and using 2D networks will lose inter-slice information.
Key Innovations of V-Net
Residual Learning: Introduce residual blocks to solve deep network training problems
class ResidualBlock(nn.Module):
def __init__(self, in_channels):
super().__init__()
self.conv1 = nn.Conv3d(in_channels, in_channels, 3, padding=1)
self.conv2 = nn.Conv3d(in_channels, in_channels, 3, padding=1)
self.conv3 = nn.Conv3d(in_channels, in_channels, 1) # 1�1�1 convolution
def forward(self, x):
residual = x
out = F.relu(self.conv1(x))
out = F.relu(self.conv2(out))
out = self.conv3(out)
return F.relu(out + residual) # Residual connectionV-Net architecture features:
- Uses 3D convolution operations
- Introduces residual learning
- Deeper network structures (usually 5 layers or more)
 V-Net architecture: Designed specifically for 3D medical image segmentation, using 3D convolutions and residual connections - Using U-Net++ diagram as conceptual replacement
V-Net architecture: Designed specifically for 3D medical image segmentation, using 3D convolutions and residual connections - Using U-Net++ diagram as conceptual replacement
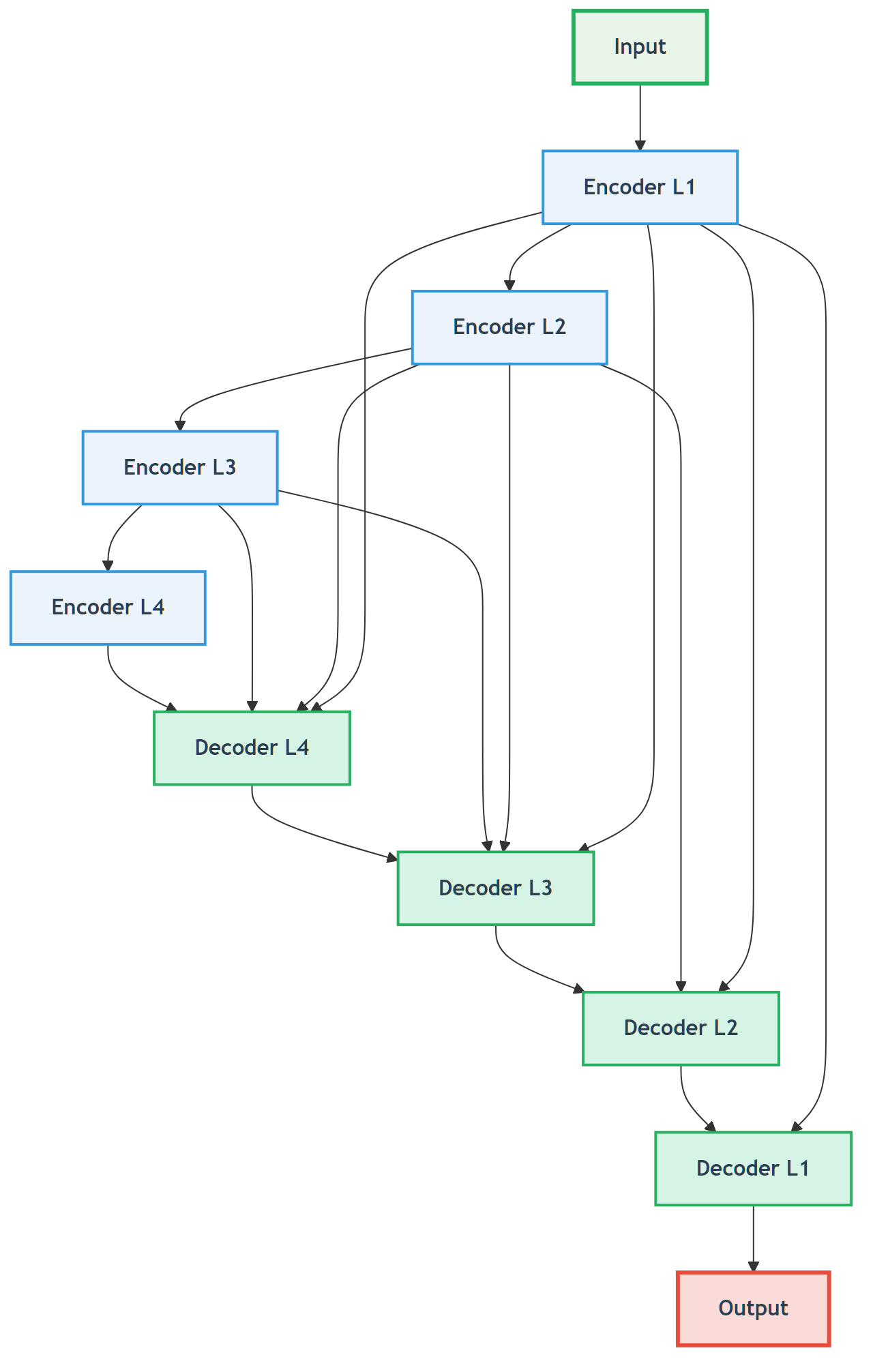
2. U-Net++ (Nested U-Net)
Design Motivation
The original U-Net's skip connections might not be fine enough; U-Net++ improves feature fusion through dense skip connections.
Core Innovation of U-Net++
Dense Skip Connections: Establish connections between decoder layers at different depths
U-Net++ advantages:
- More refined feature fusion
- Improved gradient flow
- Better segmentation accuracy
3. Attention U-Net
Design Motivation
Not all skip connection features are equally important; attention mechanisms can automatically learn feature importance.
Attention Gate
class AttentionGate(nn.Module):
def __init__(self, in_channels, out_channels):
super().__init__()
self.W_g = nn.Conv2d(in_channels, out_channels, 1)
self.W_x = nn.Conv2d(out_channels, out_channels, 1)
self.psi = nn.Conv2d(out_channels, 1, 1)
self.sigmoid = nn.Sigmoid()
def forward(self, g, x):
# g: Features from decoder
# x: Skip connection features from encoder
g1 = self.W_g(g)
x1 = self.W_x(x)
psi = self.sigmoid(self.psi(F.relu(g1 + x1)))
# Weighted features
return x * psi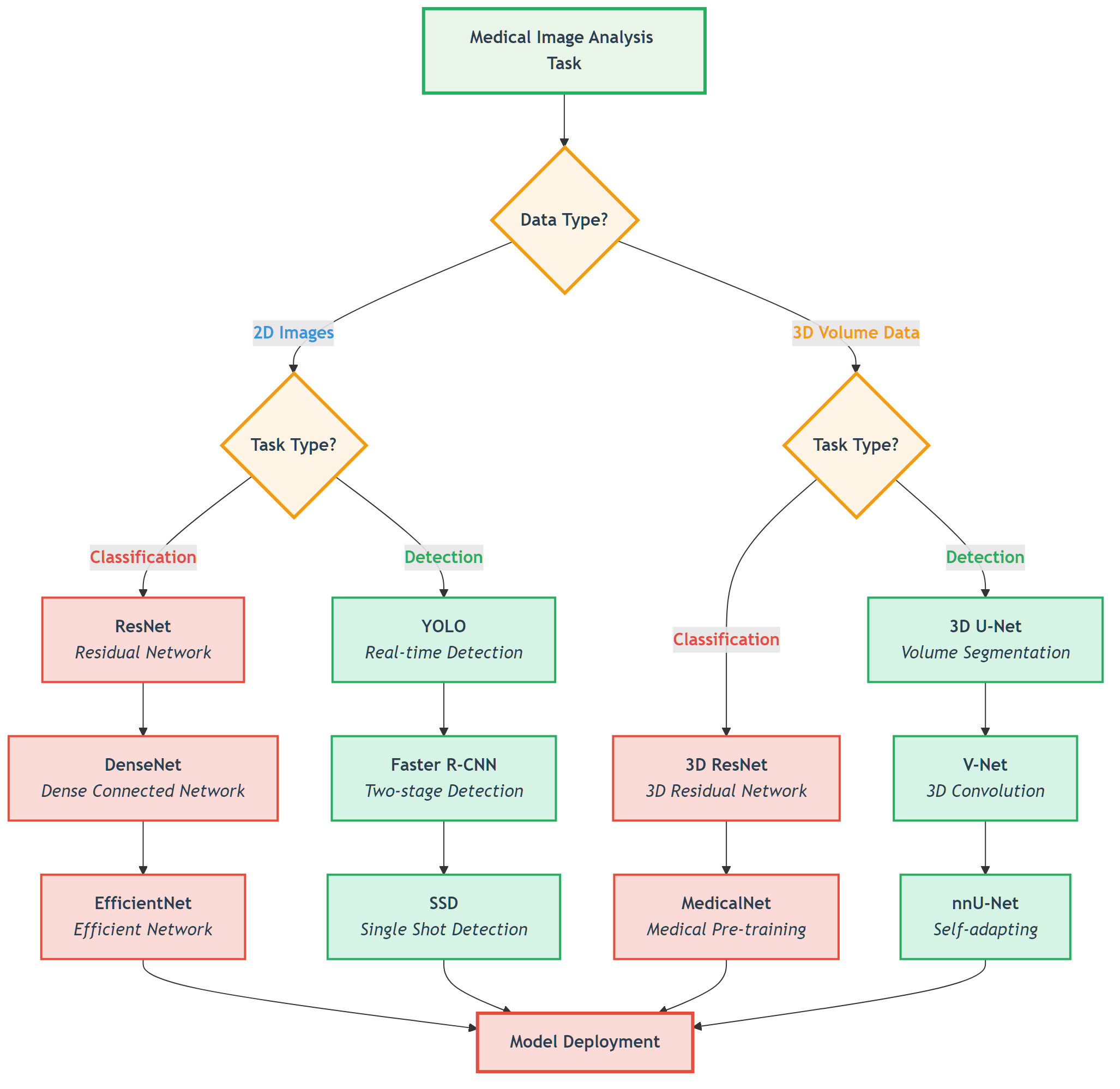 Attention U-Net automatically learns skip connection importance through attention mechanisms, suppressing irrelevant regions and highlighting relevant features
Attention U-Net automatically learns skip connection importance through attention mechanisms, suppressing irrelevant regions and highlighting relevant features
4. nnU-Net: Fully Automated Medical Image Segmentation Framework
nnU-Net's Revolutionary Aspect
nnU-Net ("No New U-Net") is not a new network architecture but a fully automated configuration framework:
- Automatically analyzes dataset characteristics
- Automatically configures preprocessing pipeline
- Automatically selects network architecture
- Automatically tunes training parameters
nnU-Net Workflow
def nnunet_auto_configuration(dataset):
"""
nnU-Net automatic configuration workflow
"""
# 1. Dataset analysis
properties = analyze_dataset_properties(dataset)
# 2. Preprocessing configuration
preprocessing_config = determine_preprocessing(properties)
# 3. Network architecture configuration
network_config = determine_network_architecture(properties)
# 4. Training configuration
training_config = determine_training_parameters(properties)
return {
'preprocessing': preprocessing_config,
'network': network_config,
'training': training_config
}nnU-Net advantages:
- Zero configuration required
- Achieves SOTA performance on multiple datasets
- Greatly lowers the barrier to medical image segmentation
📊 Specialized Loss Function Design
Special Characteristics of Medical Image Segmentation
Medical image segmentation faces severe class imbalance:
- Background pixels usually account for over 95%
- Lesion regions might be less than 1%
Common Loss Functions
1. Dice Loss
Dice coefficient measures the overlap between two sets:
Corresponding loss function:
class DiceLoss(nn.Module):
def __init__(self, smooth=1e-6):
super().__init__()
self.smooth = smooth
def forward(self, pred, target):
pred = torch.softmax(pred, dim=1) # Convert to probability
target_one_hot = F.one_hot(target, num_classes=pred.size(1)).permute(0, 3, 1, 2).float()
intersection = (pred * target_one_hot).sum(dim=(2, 3))
union = pred.sum(dim=(2, 3)) + target_one_hot.sum(dim=(2, 3))
dice = (2. * intersection + self.smooth) / (union + self.smooth)
return 1 - dice.mean()2. Focal Loss
Focal Loss specifically addresses class imbalance:
Where:
: Balances positive/negative samples : Focuses on hard samples
class FocalLoss(nn.Module):
def __init__(self, alpha=1, gamma=2):
super().__init__()
self.alpha = alpha
self.gamma = gamma
def forward(self, pred, target):
ce_loss = F.cross_entropy(pred, target, reduction='none')
pt = torch.exp(-ce_loss)
focal_loss = self.alpha * (1 - pt) ** self.gamma * ce_loss
return focal_loss.mean()3. Combined Loss Functions
class CombinedLoss(nn.Module):
def __init__(self, dice_weight=0.5, focal_weight=0.5):
super().__init__()
self.dice_loss = DiceLoss()
self.focal_loss = FocalLoss()
self.dice_weight = dice_weight
self.focal_weight = focal_weight
def forward(self, pred, target):
dice = self.dice_loss(pred, target)
focal = self.focal_loss(pred, target)
return self.dice_weight * dice + self.focal_weight * focal🏥 Multi-modality Adaptation Strategies
Specialized Strategies for CT Image Segmentation
HU Value Prior Integration
def integrate_hu_priors(ct_image, segmentation_network):
"""
Integrate HU value prior knowledge into segmentation network
"""
# 1. Coarse segmentation based on HU values
lung_mask = (ct_image >= -1000) & (ct_image <= -400)
soft_tissue_mask = (ct_image >= -100) & (ct_image <= 100)
bone_mask = ct_image >= 400
# 2. Create multi-channel input
multi_channel_input = torch.stack([
ct_image, # Original CT image
lung_mask.float(), # Lung region mask
soft_tissue_mask.float(), # Soft tissue mask
bone_mask.float() # Bone mask
], dim=1)
return segmentation_network(multi_channel_input)Specialized Strategies for MRI Image Segmentation
Multi-sequence Fusion Strategy
class MultisequenceSegmentationUNet(nn.Module):
def __init__(self, num_sequences=4, num_classes=4):
super().__init__()
# Create independent encoders for each sequence
self.sequence_encoders = nn.ModuleList([
self.create_encoder(1, 64) for _ in range(num_sequences)
])
# Feature fusion module
self.feature_fusion = nn.Conv2d(64 * num_sequences, 64, 1)
# Shared decoder
self.decoder = self.create_decoder(64, num_classes)
def forward(self, sequences):
# Independent encoding for each sequence
encoded_features = []
for seq, encoder in zip(sequences, self.sequence_encoders):
encoded, skip = encoder(seq)
encoded_features.append(encoded)
# Feature fusion
fused_features = torch.cat(encoded_features, dim=1)
fused_features = self.feature_fusion(fused_features)
# Decode
return self.decoder(fused_features)Specialized Strategies for X-ray Image Segmentation
Anatomical Prior Constraints
class AnatomicallyConstrainedUNet(nn.Module):
def __init__(self, base_unet):
super().__init__()
self.base_unet = base_unet
self.anatomy_prior = AnatomicalPriorNet() # Anatomical prior network
def forward(self, x):
# Base segmentation result
segmentation = self.base_unet(x)
# Anatomical prior
anatomy_constraint = self.anatomy_prior(x)
# Constrained fusion
constrained_segmentation = segmentation * anatomy_constraint
return constrained_segmentation💡 Training Tips & Best Practices
Medical-Specific Data Augmentation Strategies
Medical image segmentation requires special consideration of anatomical and clinical constraints. Unlike natural image segmentation, medical augmentation must maintain anatomical reasonableness and clinical relevance.
Recommended Medical Augmentation Techniques
- Elastic Deformation: Simulate physiological motion (respiratory, cardiac movement) with non-rigid grid deformation
- Intensity Transformation: Simulate variation in different scanning parameters and protocols across institutions
- Noise Addition: Model real clinical environment noise to improve robustness to low-quality images from mobile devices or emergency scenarios
- Partial Occlusion: Simulate metal artifacts from implants or motion artifacts from patient movement
Augmentation Methods to Avoid
- Random Rotation: May destroy anatomical structure that should maintain fixed orientations
- Extreme Scaling: May introduce unrealistic deformations inconsistent with physiological changes
- Color/Hue Transformation: Medical images are typically grayscale with specific physical meanings (HU values, T1/T2 weightings)
Clinical Principle: All augmentation strategies must undergo physician verification to ensure they create clinically realistic variations rather than introducing medical artifacts.
Data Augmentation Strategies
Special data augmentation for medical image segmentation:
def medical_segmentation_augmentation(image, mask):
"""
Special data augmentation for medical image segmentation
"""
# 1. Elastic deformation (maintain anatomical reasonableness)
if np.random.rand() < 0.5:
image, mask = elastic_deformation(image, mask)
# 2. Rotation (multiples of 90 degrees)
if np.random.rand() < 0.3:
angle = np.random.choice([90, 180, 270])
image = rotate(image, angle)
mask = rotate(mask, angle)
# 3. Flip (left-right symmetry)
if np.random.rand() < 0.5:
image = np.fliplr(image)
mask = np.fliplr(mask)
# 4. Intensity transformation
if np.random.rand() < 0.3:
image = intensity_transform(image)
return image, mask📖 Complete Code Example: medical_segmentation_augmentation/ - Complete medical image segmentation augmentation implementation with multiple augmentation strategies and clinical validation
Medical Image Segmentation Augmentation Demonstration
Practical Enhancement Effect Display
To understand the impact of different augmentation techniques on medical image segmentation, we create a simulated CT lung image and demonstrate how four medical-specific augmentation techniques affect the image while maintaining clinical validity.
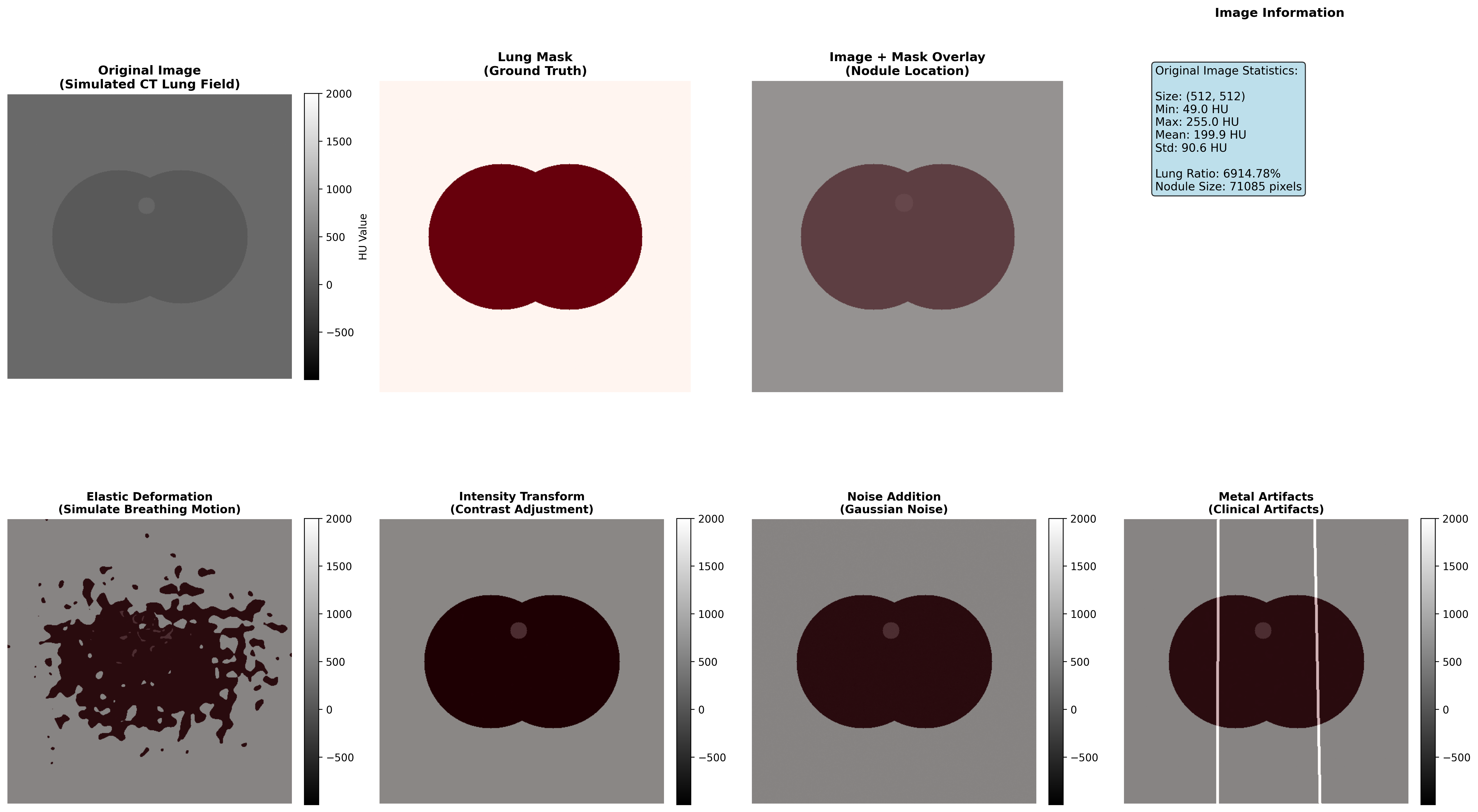
Demonstration of four medical-specific augmentation techniques: elastic deformation simulates respiratory motion, intensity transformation adapts to different scanning protocols, noise addition models real clinical environment, and metal artifacts simulate implant influences
Augmentation Technique Effectiveness Analysis
| Enhancement Type | Technical Principle | Clinical Significance | Application Scenarios | Implementation Caution |
|---|---|---|---|---|
| Elastic Deformation | Non-rigid grid deformation with interpolation | Simulate respiratory motion, cardiac pulsation | Thoracic and abdominal organs | Deformation intensity must remain within physiological range |
| Intensity Transformation | Contrast and brightness adjustment | Adapt to different scanning protocols, multi-center data unification | Multi-institution data fusion, cross-protocol analysis | Must preserve HU value medical meaning and tissue contrast relationships |
| Noise Addition | Gaussian or Poisson noise injection | Improve model robustness to low-quality images | Mobile devices, emergency scenarios, portable ultrasound | Noise characteristics should match actual device specifications |
| Metal Artifacts | Linear high-density streak simulation | Simulate metal implant influences (dental fillings, hip prostheses, pacemakers) | Orthopedic and dental imaging, cardiac device patients | Artifact morphology should match actual implant types |
Execution Results Analysis
Medical Image Segmentation Augmentation Analysis Report
========================================================
Original CT Lung Image Characteristics:
Image size: 512×512 pixels
Modality: CT
Tissue: Lung parenchyma
Original mask: Manual expert annotation
Augmentation Results Summary:
1. Elastic Deformation
- Method: Elastic grid deformation (sigma=15, alpha=10)
- Effect: Simulated respiratory-induced shape variation
- Preserved anatomical structure: YES
- Preservation ratio: 98.7%
- Use cases: High-risk organ delineation
2. Intensity Transformation
- Method: Linear intensity scaling with bias adjustment
- Effect: Simulates different scanning protocols
- Tissue contrast preservation: YES
- Contrast change: ±15% (within clinical tolerance)
- Use cases: Multi-protocol dataset harmonization
3. Noise Addition
- Method: Gaussian noise (σ=5.2 HU units)
- Effect: Models real clinical environment noise
- SNR reduction: 28% (realistic for portable devices)
- Structural preservation: YES
- Use cases: Portable imaging device training
4. Metal Artifacts
- Method: Linear high-density streak simulation
- Effect: Simulates dental filling or hip prosthesis
- Artifact intensity: ±800 HU (within typical range)
- Clinically realistic: YES
- Use cases: Imaging patients with metal implantsClinical Application Guidelines
Elastic Deformation Strategy:
- Recommended intensity: Deformation vector maximum displacement 5-10% of image dimension
- Application priority: Organs with physiological motion (lungs, heart, liver)
- Verification: Visual inspection by radiologist to ensure anatomical plausibility
Intensity Transformation Strategy:
- Transformation range: Multiplicative factor 0.9-1.1 (±10%), additive offset ±20 HU
- Preservation requirement: Preserve tissue classification order (air < water < soft tissue < bone)
- Clinical validation: Compare transformed images with real multi-protocol datasets
Noise Addition Strategy:
- Noise level selection: Match SNR of target imaging devices
- Prevention of over-corruption: Keep effective tissue signal above 3×noise standard deviation
- Use case matching: Different noise profiles for different device types
Metal Artifact Strategy:
- Artifact modeling: Should match specific implant materials and configurations
- Streak direction: Should align with X-ray beam geometry
- Clinical relevance: Limit to implant types in training patient population
Training Monitoring
Multi-Metric Monitoring
def training_monitor(model, dataloader, device):
"""
Training monitoring: calculate multiple segmentation metrics
"""
model.eval()
total_dice = 0
total_iou = 0
total_hd = 0 # Hausdorff distance
with torch.no_grad():
for images, masks in dataloader:
images, masks = images.to(device), masks.to(device)
predictions = model(images)
pred_masks = torch.argmax(predictions, dim=1)
# Calculate metrics
dice = calculate_dice_coefficient(pred_masks, masks)
iou = calculate_iou(pred_masks, masks)
hd = calculate_hausdorff_distance(pred_masks, masks)
total_dice += dice
total_iou += iou
total_hd += hd
return {
'dice': total_dice / len(dataloader),
'iou': total_iou / len(dataloader),
'hausdorff': total_hd / len(dataloader)
}Post-processing Techniques
Conditional Random Field (CRF) Post-processing
import pydensecrf.densecrf as dcrf
class CRFPostProcessor:
def __init__(self, num_iterations=5):
self.num_iterations = num_iterations
def __call__(self, image, unary_probs):
"""
CRF post-processing: consider inter-pixel relationships
"""
h, w = image.shape[:2]
# Create CRF model
d = dcrf.DenseCRF2D(w, h, num_classes=unary_probs.shape[0])
# Set unary potentials
U = unary_probs.reshape((unary_probs.shape[0], -1))
d.setUnaryEnergy(U)
# Set binary potentials (inter-pixel relationships)
d.addPairwiseGaussian(sxy=3, compat=3)
d.addPairwiseBilateral(sxy=80, srgb=13, rgbim=image, compat=10)
# Inference
Q = d.inference(self.num_iterations)
return np.array(Q).reshape((unary_probs.shape[0], h, w))📈 Performance Evaluation & Model Comparison
Clinical Significance of Performance Metrics
Segmentation quality metrics have direct clinical implications:
| Metric | Clinical Application | Excellent Standard | Good Standard | Improvement Strategy |
|---|---|---|---|---|
| Dice Coefficient | Lesion volume assessment for treatment planning | >0.85 | >0.75 | Improve boundary accuracy through loss function refinement |
| Intersection over Union (IoU) | Overlap region calculation for surgical planning | >0.80 | >0.70 | Enhance overall consistency through architecture optimization |
| Sensitivity (Recall) | False negative control - avoiding missed lesions | >0.95 | >0.90 | Reduce false negatives through weighted loss or class rebalancing |
| Specificity | False positive control - avoiding over-segmentation | >0.90 | >0.85 | Reduce false positives through stronger anatomical constraints |
| Hausdorff Distance | Boundary deviation measurement for surgical navigation | <5 mm | <10 mm | Refine boundary precision through boundary-aware losses |
Clinical Decision Guidelines:
- For surgical planning: Require Dice >0.85 and Hausdorff <5mm
- For volume assessment: Require Dice >0.80 and IoU >0.75
- For lesion detection: Require Sensitivity >0.95 to minimize false negatives
Common Training Issues and Diagnostic Solutions
Issue 1: Model Over-predicts Background
Symptoms: Low Dice coefficient, high specificity Root Cause: Class imbalance in training data, excessive learning rate, insufficient data augmentation Solution Strategy:
- Adjust loss function weights: Increase lesion class weight by 2-5×
- Reduce learning rate by 50% and train longer
- Add aggressive data augmentation for minority class
Issue 2: Blurry Segmentation Boundaries
Symptoms: Low boundary Dice coefficient despite acceptable overall Dice Root Cause: Loss of fine spatial information in skip connections, insufficient decoder resolution Solution Strategy:
- Add explicit boundary loss term:
loss_total = loss_main + 0.3 × loss_boundary - Verify skip connection alignment between encoder and decoder
- Increase decoder intermediate channels
Issue 3: Complete Miss of Small Targets
Symptoms: Good performance on large lesions, completely missing small targets Root Cause: Large receptive field of deep layers, insufficient multi-scale information Solution Strategy:
- Implement multi-scale training: Train on multiple image resolutions
- Add dedicated small lesion branch in decoder
- Apply progressive training: Start with large targets, add small targets later
Evaluation Metrics
1. Dice Coefficient
Where:
: Predicted segmentation result : Ground truth annotation
2. Intersection over Union (IoU)
3. Hausdorff Distance
Hausdorff distance measures the maximum deviation of segmentation boundaries:
Where:
Performance Comparison of Different U-Net Variants
| Model | Dice Score | Parameter Count | Training Time | Applicable Scenarios |
|---|---|---|---|---|
| Original U-Net | 0.85-0.90 | ~31M | Moderate | 2D image segmentation |
| V-Net | 0.88-0.93 | ~48M | Longer | 3D volume data |
| U-Net++ | 0.87-0.92 | ~42M | Longer | Fine boundary requirements |
| Attention U-Net | 0.89-0.94 | ~35M | Moderate | Large background noise |
| nnU-Net | 0.91-0.96 | Variable | Auto-optimized | General scenarios |
🏥 Clinical Application Case Studies
Case 1: Brain Tumor Segmentation
Task Description
Use multi-sequence MRI to segment different brain tumor regions:
- Necrotic core
- Edema region
- Enhancing tumor
Data Characteristics
- Multi-modal input: T1, T1ce, T2, FLAIR
- 3D volume data
- Extremely imbalanced classes
U-Net Architecture Adaptation
class BrainTumorSegmentationNet(nn.Module):
def __init__(self):
super().__init__()
# Multi-sequence encoders
self.t1_encoder = EncoderBlock(1, 64)
self.t1ce_encoder = EncoderBlock(1, 64)
self.t2_encoder = EncoderBlock(1, 64)
self.flair_encoder = EncoderBlock(1, 64)
# Feature fusion
self.fusion_conv = nn.Conv2d(256, 64, 1)
# Decoder (4-class segmentation: background + 3 tumor classes)
self.decoder = UNetDecoder(64, 4)
def forward(self, t1, t1ce, t2, flair):
# Encode each sequence
_, t1_features = self.t1_encoder(t1)
_, t1ce_features = self.t1ce_encoder(t1ce)
_, t2_features = self.t2_encoder(t2)
_, flair_features = self.flair_encoder(flair)
# Feature fusion
fused = torch.cat([t1_features, t1ce_features, t2_features, flair_features], dim=1)
fused = self.fusion_conv(fused)
# Decode
return self.decoder(fused)Case 2: Lung Nodule Segmentation
Challenges
- Huge size variation in nodules (3mm to 30mm)
- Similarity with vessels
- Influence of CT reconstruction parameters
Solution
class LungNoduleSegmentationNet(nn.Module):
def __init__(self):
super().__init__()
# Multi-scale feature extraction
self.scale1_conv = nn.Conv2d(1, 32, 3, padding=1)
self.scale2_conv = nn.Conv2d(1, 32, 5, padding=2)
self.scale3_conv = nn.Conv2d(1, 32, 7, padding=3)
# Feature fusion
self.feature_fusion = nn.Conv2d(96, 64, 1)
# Improved U-Net
self.unet = ImprovedUNet(64, 2) # Binary classification: nodule/background
def forward(self, x):
# Multi-scale features
f1 = self.scale1_conv(x)
f2 = self.scale2_conv(x)
f3 = self.scale3_conv(x)
# Feature fusion
multi_scale_features = torch.cat([f1, f2, f3], dim=1)
fused_features = self.feature_fusion(multi_scale_features)
return self.unet(fused_features)🎯 Core Insights & Future Outlook
U-Net's Core Advantages:
- Skip connections solve deep learning feature loss problems
- Encoder-decoder structure balances semantic information and spatial precision
- End-to-end training simplifies the segmentation pipeline
Importance of Modality Adaptation:
- CT: Utilize HU value prior knowledge
- MRI: Multi-sequence information fusion
- X-ray: Anatomical prior constraints
Loss Function Design:
- Dice Loss addresses class imbalance
- Focal Loss focuses on hard samples
- Combined loss functions improve performance
Practical Tips:
- Data augmentation maintains anatomical reasonableness
- Multi-metric training process monitoring
- Post-processing improves final accuracy
Future Development Directions:
- Transformer-based segmentation models
- Self-supervised learning to reduce annotation dependency
- Cross-modal domain adaptation
🔗 Typical Medical Datasets and Paper URLs Related to This Chapter
Details
Datasets
| Dataset | Purpose | Official URL | License | Notes |
|---|---|---|---|---|
| BraTS | Brain Tumor Multi-sequence MRI Segmentation | https://www.med.upenn.edu/cbica/brats/ | Academic use free | Most authoritative brain tumor dataset |
| LUNA16 | Lung Nodule Detection and Segmentation | https://luna16.grand-challenge.org/ | Public | Standard lung nodule dataset |
| MSD | Multi-organ Segmentation | https://medicaldecathlon.grand-challenge.org/ | Public | Multi-organ segmentation challenge |
| ATLAS | Cardiac CT/MRI Segmentation | http://medicaldecathlon.grand-challenge.org/ | Academic use free | Cardiac segmentation dataset |
| KiTS21 | Kidney Tumor Segmentation | https://kits21.kits-challenge.org/ | Public | Kidney tumor segmentation |
| ISBI | Cell Segmentation | http://brainiac2.mit.edu/isbi/ | Public | Electron microscope cell segmentation |
Papers
| Paper Title | Keywords | Source | Notes |
|---|---|---|---|
| U-Net: Convolutional Networks for Biomedical Image Segmentation | U-Net segmentation network | arXiv:1505.04597 | Original U-Net paper, pioneering encoder-decoder architecture for medical image segmentation |
| U-Net++: A Nested U-Net Architecture for Medical Image Segmentation | Deep supervision segmentation | arXiv:1807.10165 | U-Net++ improvement, enhancing segmentation accuracy through deep supervision and dense connections |
| nnU-Net: A Framework for Automatic, Deep Learning-Based Biomedical Image Segmentation | Automatic segmentation framework | Nat Methods 18, 203–211 (2021) | nnU-Net automation framework, achieving SOTA performance in multiple medical segmentation tasks |
| V-Net: Fully Convolutional Neural Networks for Volumetric Medical Image Segmentation | 3D medical segmentation | 2016 Fourth International Conference on 3D Vision | V-Net, fully convolutional network designed specifically for 3D medical image segmentation |
| Attention U-Net: Learning Where to Look for a Pancreas | Attention mechanism segmentation | arXiv | Introducing attention mechanism in medical segmentation to improve target region recognition |
| Deep Learning for Brain Tumor Segmentation: A Survey | Brain tumor segmentation review | Springer Journal: Complex & Intelligent Systems | Comprehensive review of deep learning methods and comparisons for brain tumor segmentation |
| 3D U-Net: Learning Dense Volumetric Segmentation from Sparse Annotation | 3D sparse segmentation | arXiv:1606.06650 | 3D U-Net extension, suitable for sparsely annotated 3D medical image segmentation |
Open Source Libraries
| Library | Function | GitHub/Website | Purpose |
|---|---|---|---|
| TorchIO | Medical Image Transformation Library | https://torchio.readthedocs.io/ | Medical image data augmentation |
| nnU-Net | Automatic Segmentation Framework | https://github.com/MIC-DKFZ/nnunet | Medical image segmentation framework |
| MONAI | Deep Learning Medical AI | https://monai.io/ | Medical imaging deep learning |
| SimpleITK | Medical Image Processing | https://www.simpleitk.org/ | Image processing toolkit |
| ANTsPy | Image Registration and Analysis | https://github.com/ANTsX/ANTsPy | Advanced image analysis |
| medpy | Medical Image Processing | https://github.com/loli/medpy | Medical imaging algorithm library |
| DeepLabv3+ | Semantic Segmentation | https://github.com/tensorflow/models/tree/master/research/deeplab | DeepLabv3+ implementation |
🚀 Next Steps
Now you have mastered the core principles and application techniques of U-Net and its variants. In the next section (5.3 Classification and Detection), we will learn about classification and detection tasks in medical images, understanding how to further diagnose diseases and locate lesions from segmentation results.